My Experience with Postpartum Depression
May is Mental Health Awareness Month. Mental Health is important because YOU are important and YOU are made up of body, mind, soul, and emotions. All these things work together, and when one part struggles, everything else is a bit off-key too. Mental Health is a big buzzword right now- there’s so much covered under the umbrella of the term, so I want to focus on Postpartum Depression specifically.
 According to the Centers for Disease Control, Postpartum Depression affects 1 in 8 women. It looks different, feels different, and hits at different times. Postpartum Depression wants us to be afraid and ashamed and I think that’s total crap. I’m here to talk about what I experienced with Postpartum Depression (PPD).
According to the Centers for Disease Control, Postpartum Depression affects 1 in 8 women. It looks different, feels different, and hits at different times. Postpartum Depression wants us to be afraid and ashamed and I think that’s total crap. I’m here to talk about what I experienced with Postpartum Depression (PPD).
My doctor warned me and told me about the signs of PPD. I had struggled with depression my whole life, so I thought I knew what signs to look for. That first night with my very first baby, I panicked. I couldn’t get her to stop crying, I had no idea what to do, and my husband was sound asleep. I made the nurse help me. The next night, baby and I were up all night by ourselves at home, and she didn’t stop crying no matter what I did. She cried every time I put her down, so I held her. I held her for 4 months straight.
Lack of sleep contributes to PPD.
Stress contributes to PPD.
My daughter had problems eating, and I was trying everything to breastfeed. One feed would take nearly an hour, and we would both end up crying, feeling defeated afterwards, only to have to relive the same experience an hour later.
Guilt contributes to PPD.
Fear contributes to PPD.

Three days after my daughter was born, I stopped sleeping. I started being afraid of anything and everything, so I wouldn’t let her out of my sight and couldn’t put her down. I imagined horrible things happening, and at 2 in the morning, any sound in the house led me to imagine our house would fall into a sinkhole as we were running away from some intruder.
My postpartum converted into postpartum anxiety and evolved into psychosis. This all happened in the span of one week.
There weren’t tons of tears. There were giggles and snuggles. There weren’t typical signs. My husband knew something was off and told me to speak to my doctor. There weren’t signs to me, but there were big issues that only the person closest to me saw.
My OBGYN prescribed me something to help me sleep, and then I saw a psychiatrist that same week to discuss an antidepressant that would be safe for me to use while I was breastfeeding.
But nothing changed, even when I did what they told me to do.
- I walked and exercised every single day.
- I joined a mom’s group.
- I reached out to friends.
- I worked a part-time job.
We kept trying different medications, different strategies, and counseling multiple times a week, but nothing changed. I even stopped breastfeeding to try different things, and I couldn’t find relief. What was happening and why did having a baby, which was the best thing to ever happen to me, make me feel so……
Hopeless?
Postpartum depression makes you feel hopeless. It can also make you feel:
- Sad
- Overwhelmed
- Anxious
- Thoughts of hurting yourself or your baby
- Uninterested in baby
- Unable to sleep
- Like a bad parent
- Like you don’t love your baby
- Disconnected from your baby
Unfortunately, I didn’t get to find a solution for my depression. I worked really hard to get better, and after 8 months, I found out I was pregnant and had to stop taking my medication. But my hormones shifted, and I did feel so much better. Looking back, it was probably hormone therapy that I needed and not antidepressant medication.
The cause of postpartum depression is not fully known, making it hard to determine how to solve and treat the problem. There’s no one-size-fits-all solution. And the other thing… all of the contributing factors to what is thought to cause PPD are out of our control. Things like genetic predisposition or a history of depression in the past, hormone levels, and psychosocial stressors are all thought to be factors that play a potential role in creating PPD. Sometimes there’s so many other conditions and things that can come up mental health- wise after giving birth.
I wanted to help make people aware that it’s not just you. You’re not alone. You’re not a bad mom. You’re not crazy. You’re not wrong. Your feelings are not wrong. Your body is not wrong. You are you, and you’re doing a great job. You woke up this morning. You did something that some people will never be able to do: you grew a human life! You ARE a human life that is beyond valuable. So even though things may feel terrible, feelings lie. It won’t be this way forever, and you are killing it.
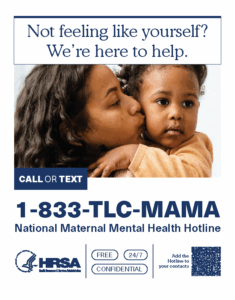
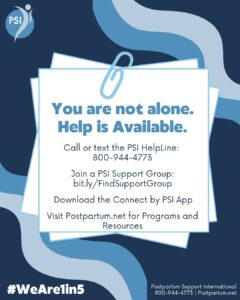
Sometimes we all need help. Especially after having a baby! If you don’t have the village it takes to raise a baby or feel your need for help is beyond what your friends and family can offer, here are some free resources. Don’t do this alone. If you or someone you know is struggling with depression or thoughts of suicide, there are people who care and want to help. Please tell your doctor that you are struggling and want to get help with what may be postpartum depression.
- National Maternal Mental Health Hotline 1-833-TLC-MAMA (1-833-852-6262). Free, confidential, 24/7 mental health support for moms and their families before, during, and after pregnancy. (English & Spanish)
- 988 Suicide & Crisis Lifeline – If you need to talk, the 988 Lifeline is here. At the 988 Suicide & Crisis Lifeline, we understand that life’s challenges can sometimes be difficult. Whether you’re facing mental health struggles, emotional distress, alcohol or drug use concerns, or just need someone to talk to, our caring counselors are here for you. You are not alone.
- Postpartum Support International – Call the PSI HelpLine: 1-800-944-4773, #1 En Español or #2 English. Text “Help” to 800-944-4773 (EN). Text en Español: 971-203-7773. The PSI HelpLine does not handle emergencies. HelpLine hours are 8am-11pm EST. Services are in English and Spanish.People in crisis should call their local emergency number or the Suicide & Crisis Lifeline.
- Well Mama- Mental Support for Parents and Caregivers Text SUPPORT to 541-525-0495 for Support or Info. WellMama is a non-profit organization that provides comprehensive pregnancy and postpartum support for new, expectant, and grieving parents.
- Pollywog Mental Health Resources for Families